When the three hottest months of the high-sun season roll around, many Canadians are used to dealing with pests - be it those pesky mosquitoes when working out in the yard or sticky ticks when walking in the forest. But in a warming world, these pests are becoming more than just a nuisance for Canadians.
Infectious diseases carried by insect vectors such as ticks are increasingly common in parts of Canada, due in part to climate change.
One tick-borne disease of particular importance to the health of Canadians is Lyme disease, which is most commonly spread by blacklegged ticks (also known as deer ticks).
Read more: What is Lyme Disease?
Lyme disease is an illness caused by bacteria spread by blacklegged ticks. The bacteria can be carried by animal hosts - such as birds, mice, and deer - and then transmitted to humans when a tick bites an infected animal and then bites a person. Blacklegged ticks are most active in spring and summer, and generally found in forests, wooded areas, shrubs, tall grass and leaf piles.[1]
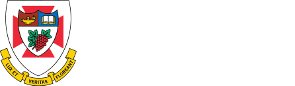
Though it is relatively new in Canada, Lyme disease is increasingly a health concern that Canadians should be aware of. The map below from the Public Health Agency of Canada shows Lyme disease risk areas as of 2016, based on reported human cases as well as field surveillance. Experts also note that ticks are spreading outside of these risk areas -- moving into new habitats at a rate of 35-55 km per year -- so lower levels of risk do exist in other areas.
Lyme disease risk area map, from the Public Health Agency of Canada [1]
Though he spends his summers out cutting wood for his home in rural Manitoba, Rick Holmes hadn’t thought much about Lyme disease. But one day, after being out in the bush the weekends prior, he started feeling sick.
“I was just achey and inflamed all over. I had these big rash spots all over me, a big one on my leg, kind of all over my back…” Rick explained. “It wasn't really evident what was the root cause of my sickness at that time.” After receiving tests at several hospitals over the course of a few weeks, Rick was eventually diagnosed with Lyme disease.

Read more: What does a blacklegged tick look like?
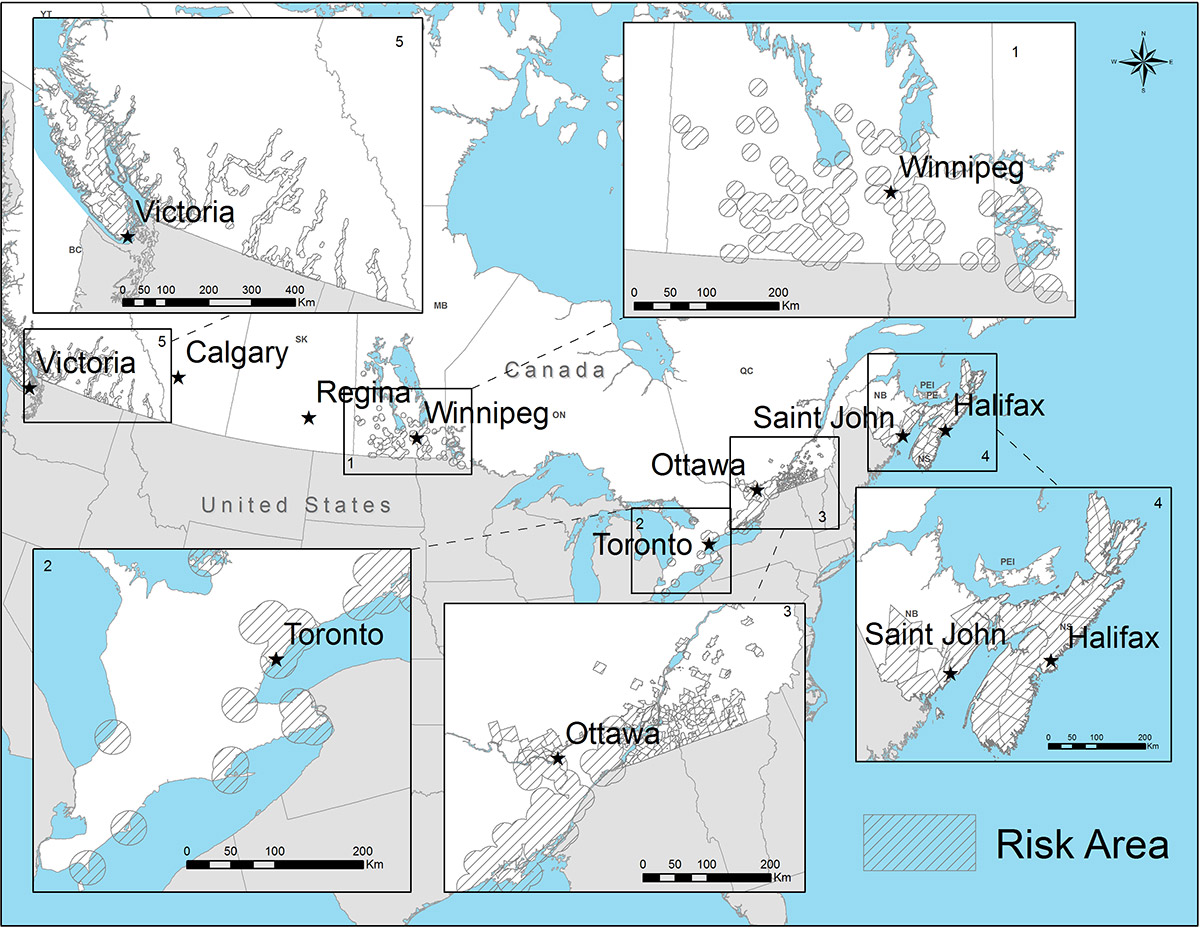
If you get bitten by a tick, it is important to be able to identify the type of tick to know if it may carry Lyme disease. Blacklegged ticks are different sizes at different points in their life cycle. The spring and early fall are peak times for adults, while in midsummer you’re more likely to come across the ticks in earlier stages of development called nymphs.
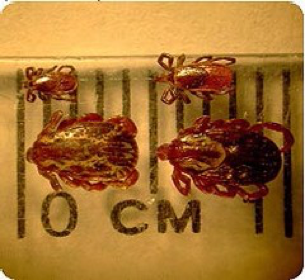
Fig 1. Unfed adult blacklegged ticks (top) vs American dog (wood) ticks (bottom). In comparison to other common tick species such as the American dog tick, blacklegged ticks are smaller and have no markings on their backs.

Fig 2. Adult female blacklegged ticks in different stages of feeding. As the tick feeds, it takes in blood from the host and grows in size. The longer it has been attached, the larger it becomes.

Fig 3. Nymph blacklegged ticks at different stages of feeding. The nymphs are much smaller than adults, and harder to spot if they are attached, but they can still carry and transmit the disease. Luckily, nymphs are less likely to bite humans than adult ticks.
Figures from Health Canada[2]
Climate change is increasing spread of ticks and Lyme disease
Stories like Rick’s are increasingly common in Canada. Over the past few decades, as blacklegged ticks have been spreading northward into new territory, reported cases of Lyme disease have grown from about 150 in 2009 to over 2,000 in 2017. [3]
Scientist Robbin Lindsay of the National Microbiology Laboratory in Winnipeg “had a front row seat to the emergence of blacklegged ticks in Canada.”
Lindsay and his team have been monitoring these ticks since they first arrived in southern Ontario in the 1990s. They’ve been tracking their spread north and westward, and finding that people are now being exposed to Lyme disease in regions where they weren’t before.
“We see essentially an epidemic of Lyme disease in Canada and in North America, a changing range that is driven in part by a warming climate that has allowed these ticks to invade into new environments,” described Lindsay.
Watch Dr. Robbin Lindsay and other experts working at the forefront of the spread of Lyme disease in our video A Ticking Clock: Lyme disease, climate change, and public health.
How does climate change impact tick populations? Longer, hotter summers and more mild winters increase the ticks’ rates of survival, growth and reproduction. This means that they can survive and establish populations in areas where they previously couldn’t, and increase their numbers where they were already established. Longer summers also mean a longer season where ticks are active and people are outdoors - increasing the window of opportunity for the two to meet.
Additionally, climate change is expected to increase the range, abundance, and activity of rodent, bird, and deer hosts that carry the disease. These hosts are critical for the ticks to move through their lifecycle and can facilitate tick travel over long distances.
Monitoring and mapping the spread of ticks
Because of these impacts of climate change, it’s important to be able to predict how ticks and disease may spread in years to come so that we can prepare and adapt.
Lindsay and his team are working with scientist Nicholas Ogden of the Public Health Agency of Canada to model the spread of ticks under climate change. Lindsay’s team in Winnipeg shares tick data with Ogden in St. Hyacinthe, Quebec, who uses it to map areas of risk. Creating risk maps of where the disease is now, and where it might appear in the future, can help develop policies and strategies for public health.
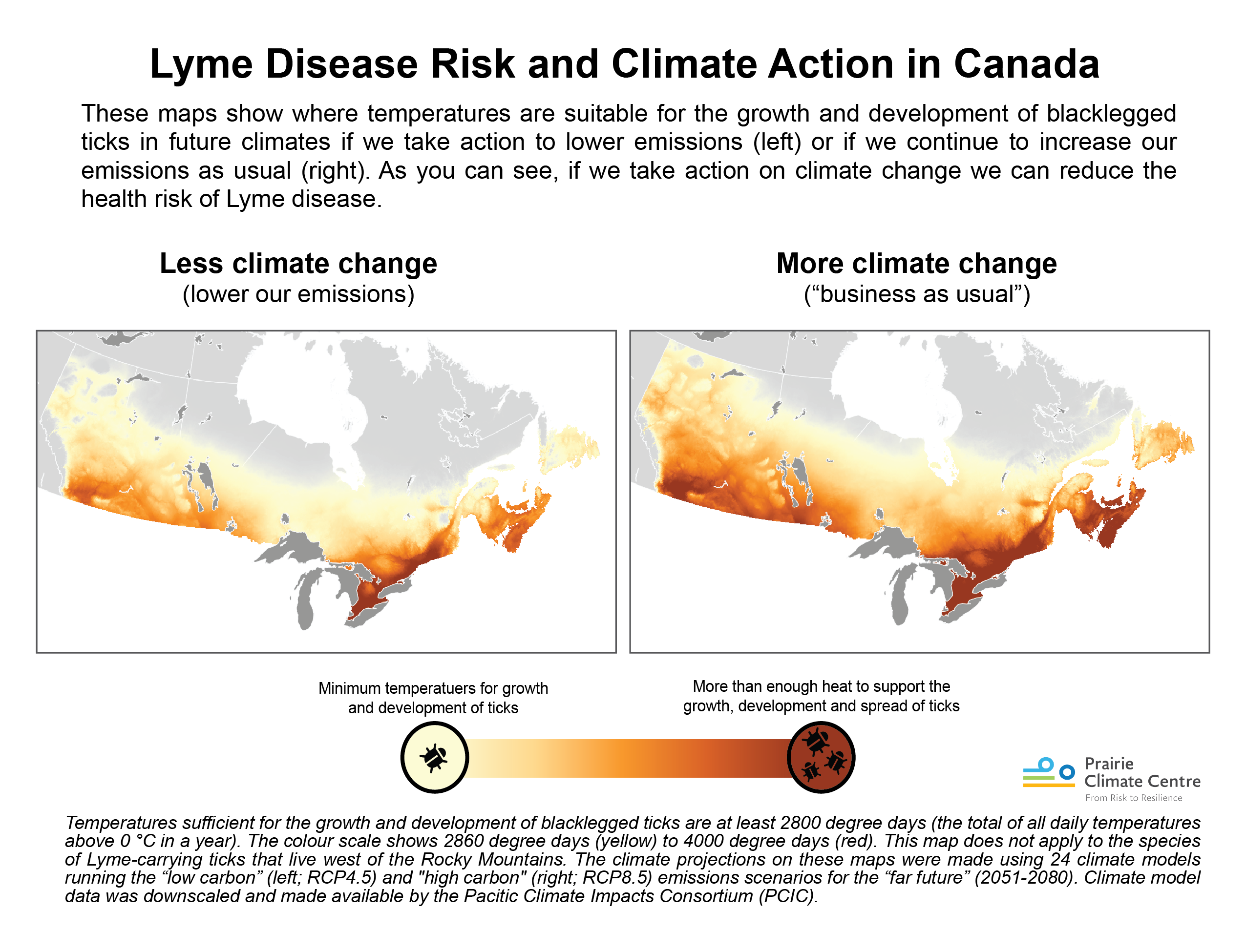
The maps below visualize the potential increasing range of ticks over the next 30-60 years under a “business as usual” scenario [4] spreading as far as Newfoundland & Labrador, and north in Ontario and Manitoba up to Hudson Bay.
These maps are based on temperatures suitable for the survival and reproduction of blacklegged ticks, which can carry Lyme disease. However, warming temperatures is not the only factor affecting the movement and range of blacklegged ticks.
They are also influenced by things such as movement of animal hosts, changes to habitat through deforestation and reforestation, migratory patterns of birds, and more. And because these different factors all act together with each other, it is difficult to predict exactly where and how fast the ticks will spread.
Read more: Tracking the ticks
One way that scientists test and refine these risk maps is by going out and collecting ticks in certain areas and comparing them to the maps. Kateryn Rochon, a researcher and professor at the University of Manitoba, spends a lot of her time out in the field with her students looking for ticks.
“It’s important to do surveillance because not only will we get information on where the ticks are,” says Rochon, “we’ll also find areas where the ticks may not be now, but the conditions are suitable, so that you can say ‘this is a place we need to watch’.”

Dr. Kateryn Rochon and her student sampling for blacklegged ticks in a park near Winnipeg, MB.
Read more: If I’ve been bitten by a tick, do I have Lyme disease?
Ticks are nothing new to many Canadians. It is important to remember that there are many different species of ticks, which have been living in parts of Canada for a long time. What’s new are two specific species of tick - the blacklegged or deer tick (Ixodes scapularis) in central and eastern Canada, and the western blacklegged tick (Ixodes pacificus) in British Columbia - which can carry the bacteria that causes Lyme disease. These are the potential troublemakers.
Not all blacklegged ticks are infected with the Lyme bacteria however. In fact, not even the majority. It is estimated that on average about 20% of blacklegged ticks carry the disease [5], though in some areas that can be much higher, up to 60-75%[6].
If you are bitten by an infected tick, you aren’t guaranteed to get the disease. The tick must be attached for 24-36 hours to transmit the disease[7].
As Dr. Lindsay summarizes, “you get Lyme disease when three things happen: you’re bitten by the right type of tick; that tick has been infected with the agent of Lyme disease; and it’s been attached long enough to transmit.”
If bitten, you are advised to remove the tick slowly and carefully with tweezers, and keep the tick to bring to a medical professional if any symptoms ensue. You can also submit ticks for identification and to help researchers’ efforts of tracking their spread. For more details and instructions on removing and submitting a tick, visit Health Canada’s webpage.
How to prevent Lyme disease
While Lyme disease is increasing in Canada, many experts say this shouldn’t deter people from going outside.
"I think it's important to still go outside, and not be afraid of going outside," says Rochon. "You just need to adapt your behavior, protect yourself, and be aware of the risks.”
There are some straightforward actions you can take to reduce your chance of a tick bite.
The Public Health Agency of Canada (PHAC) and Health Canada recommend these preventative measures when travelling into areas with risk of Lyme disease, including [7]:
- Apply treatments of the insecticide permethrin to clothing to repel ticks when travelling to highly Lyme endemic areas
- Wear light coloured long-sleeved clothing, tucking in shirts and pants
- Stay on cleared paths when walking or hiking
- Shower within several hours of being in the forested area and do daily tick checks on yourself and your children (particularly in hair, underarms, around ears, behind the knees, between the legs and around the waist).
- Remove any found ticks immediately. Removing within 24 hours can help prevent infection.
- Check your outdoor gear and clothing for ticks. To ensure they aren’t carrying ticks, dry them on high heat and/or wash in hot water to remove any that may be remaining.
It is also important to stay informed about the Lyme disease risk areas, where you live, work, and travel. PHAC keeps an updated list of places in each province where blacklegged tick populations are known, as well as regional risk maps, which can be found here[1].
Read more: The challenges of Lyme disease diagnosis
One of the challenging things about diagnosing Lyme disease is that the symptoms can vary from person to person and are sometimes non-specific. Many people experience flu-like symptoms, such as fatigue, fever, headache, and hot and cold sweats. The majority of people will develop a rash around the area of the tick bite - sometimes in the shape of the well-known “bullseye.”
Lunenburg doctor Cecilia Newton sees patients with concerns of Lyme disease every day in her clinic. “Most commonly we’ll see the bullseye rash… It’s a flat, red, expanding rash that’s specific to the disease,” describes Newton. “In the minority of cases, we’ll have patients come in with atypical symptoms and signs that can often mimic other illnesses… And the diagnosis in that case can be quite challenging.”
In unusual cases, if the disease is undetected and left untreated for several months, symptoms such as joint pain, neurological problems, and cardiac issues may arise, and the illness can become debilitating in some cases[8]. These symptoms are sometimes mistaken for arthritis, heart problems, or other health issues - and vice versa - making Lyme diagnosis difficult.
Diagnosis is further complicated by the fact that in regions where the disease is new, people are often unfamiliar with Lyme[9]. Many Canadians report being misdiagnosed when first seeking medical help, and some have even travelled to the US to seek treatment, where the disease is more common and has been around for longer. Part of the challenge is that blood tests for Lyme disease are more or less accurate, depending on when the tests are given and how the bacteria has spread in the body [10].
At the same time, awareness, testing, and treatment for Lyme disease has increased substantially in Canada over the past several years. Once a person is diagnosed with Lyme disease, they can usually be treated successfully with antibiotics [11]. If you feel any flu-like symptoms or develop a rash after being outside, and think you may have been in contact with a tick, the safest bet is to go to your doctor.
Climate change and disease mitigation
While the critical work needed to adapt to the rising spread of Lyme disease is underway, we must not forget to also ask - how can we slow the spread of these ticks?
We know that Lyme-infected ticks are spreading and will continue to do so in the near future under existing climate change. But we can take measures to stop Lyme and other insect-borne diseases from spreading even further by acting to mitigate use of fossil fuels and the associated greenhouse gases that cause climate change.
As you can see by looking at the comparative maps below, by reducing our emissions we can reduce associated temperatures that allow the spread of blacklegged ticks. If we curb our emissions, less of the country will be exposed to the ticks that carry Lyme disease, and that means less infectious disease for Canadians. In other words, by acting on climate change we can actually reduce risks to public and environmental health.
By reducing our “emissions pathway” we’re also likely to create health “co-benefits” because our communities will be more walkable, have better public transit, more resilient infrastructure, and more green spaces that promote wellness. By lowering greenhouse gases, we also lessen the likelihood wildfires, heatwaves, and extreme weather all linked to changing climate.
The rise of Lyme disease and other infectious diseases are just a few examples of the many ways that climate change is increasingly impacting our lives. Although it will take an urgent and unparalleled collective effort among government, industry, communities, and individuals to scale the solutions that we need to address these issues, it is indeed possible.
You can read more about the connections between climate change and health, and the co-benefits of solutions, in our Climate Change and Health and Take Action articles.
References
- https://www.canada.ca/en/public-health/services/diseases/lyme-disease/risk-lyme-disease.html
- https://www.canada.ca/en/health-canada/services/pest-control-tips/blacklegged-deer-ticks.html
- https://www.canada.ca/en/public-health/services/diseases/lyme-disease/surveillance-lyme-disease.html
- "Business as usual" here refers to a high carbon scenario (RCP8.5) in which emissions continue to grow at the current rate. For more information on emissions scenarios and the climate modeling used here, visit https://climateatlas.ca/glossary
- https://www.brandonsun.com/westman-this-week/lyme-disease-carrying-ticks-return-483597563.html
- https://www.cbc.ca/news/canada/thunder-bay/lyme-disease-corkscrew-island-1.3878034
- https://www.canada.ca/en/public-health/services/diseases/lyme-disease/prevention-lyme-disease.html
- https://www.canada.ca/en/public-health/services/diseases/lyme-disease/symptoms-lyme-disease.html
- https://www.nationalobserver.com/2018/03/07/news/ticks-creep-canada-bringing-lyme-disease-and-confusion-them
- Van Hout, M. C. (2018). The Controversies, Challenges and Complexities of Lyme Disease: A Narrative Review. Journal of Pharmacy & Pharmaceutical Sciences, 21(1), 429-436. https://doi.org/10.18433/jpps30254
- https://www.canada.ca/en/public-health/services/diseases/lyme-disease/treatment-lyme-disease.html
Recommended Article Citation
Climate Atlas of Canada. (n.d.) Lyme Disease Under Climate Change. Prairie Climate Centre. https://climateatlas.ca/lyme-disease-under-climate-change







.png)